More than 80 per cent of hospitalized COVID-19 patients had vitamin D deficiency: study
TORONTO — More than 80 per cent of COVID-19 patients at a hospital in Spain had a vitamin D deficiency, according to a new study.
Researchers at the University Hospital Marques de Valdecilla in Santander, Spain looked at the vitamin D levels of 216 patients admitted to hospital for coronavirus treatment between March 10 and March 31.
For the study, the 216 hospitalized patients’ vitamin D levels were compared to those of a control group of 197 people of similar age and sex from a population-based cohort in the same geographical area.
Of the 216 hospitalized patients, 19 who had been taking oral vitamin D supplements for more than three months before their admissions were analyzed as a separate group.
The researchers found that 82 per cent of the hospitalized COVID-19 patients (who were not taking supplements) were vitamin D deficient, while 47 per cent of the control group had the same deficiency.
The study also noted that vitamin D levels were “especially lower” in men with COVID-19 compared to women.

Dr. Jose Hernandez, a co-author of the study and an associate professor of neurophysiology at the University of Cantabria in Spain, said there are many factors that could explain why men with COVID-19 had lower vitamin D levels than women, including lifestyle or dietary habits and different comorbidities.
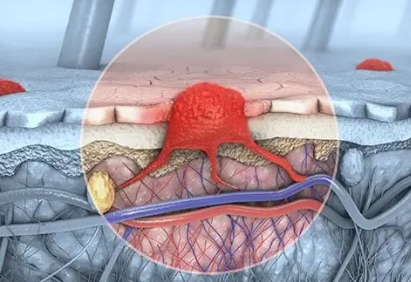
The study’s authors were particularly interested in studying vitamin D because they said there’s evidence to suggest it plays a role in COVID-19 infection. Vitamin D is a hormone produced by the kidneys, which controls blood calcium concentration and affects the function of the immune system.
Vitamin D deficiency has also been linked to health concerns including heart disease, diabetes, cancer, and multiple sclerosis.
According to the study, there is also “compelling evidence” for an epidemiological association between low levels of vitamin D and infections such as influenza, HIV, and the hepatitis C virus.
“There are numerous pieces of evidence in the literature that support the beneficial effect of vitamin D on the immune system, especially regarding protection against infections, including viral infections,” Hernandez said in an email to CTVNews.ca on Sunday.
While the researchers reported a higher prevalence of vitamin D deficiency in hospitalized COVID-19 patients compared to the control group, they did not find an association between vitamin D levels and the severity of the disease, such as the need for ICU admission, mechanical ventilation, or even death.
And, although they didn’t establish an association between vitamin D deficiency and the severity of COVID-19, the study’s authors noted that the group of hospitalized patients who had been taking oral supplements prior to admission had slightly more favourable outcomes than those who didn’t take supplements before they were admitted to hospital, including lower ferritin levels, a decreased need for the immunosuppressive drug tocilizumab, and lower ICU admissions.
The study found that patients with a vitamin D deficiency also had raised serum levels of inflammatory markers, such as ferritin and D-dimer.
“The most severe forms of COVID-19 are characterized by a hyperinflammatory state, the so-called ‘cytokine storm,’ that occurs over the first week of symptoms’ onset, and led to acute respiratory distress syndrome and other organ complications causing increased mortality,” Hernandez explained.
“We found that COVID-19 patients with lower serum vitamin D levels had raised serum ferritin and D-dimer levels, which are markers of this hyperinflammatory response.”
In addition to not establishing a relationship between low levels of vitamin D and the severity of COVID-19, including mortality, the study’s authors also acknowledged their research doesn’t show that vitamin D deficiency is a risk factor for contracting the disease.
“We must wait for the results of the ongoing large and properly designed studies to determine whether vitamin D can prevent SARS-COV-2 infection, or reduce its severity,” Hernandez said.
Given the safety and low cost of vitamin D treatments, Hernandez said it would be reasonable to treat those who are most at risk of vitamin D deficiency, such as seniors and those with comorbidities, and who also happen to be the most at risk for developing severe outcomes from COVID-19.
The study was published in the Endocrine Society’s “Journal of Clinical Endocrinology & Metabolism” on Tuesday. https://academic.oup.com/jcem/advance-article/doi/10.1210/clinem/dgaa733/5934827




Leave a Reply
You must be logged in to post a comment.